Flying with a sinus infection can transform an exciting trip into a painful ordeal. The pressure changes during takeoff and landing often exacerbate sinus discomfort, leading many to dread air travel when congested. But is flying with a sinus infection always a bad idea? And if you must fly, what can you do to minimize the pain?
Understanding why sinus infections cause in-flight pain is the first step to managing it. The discomfort isn’t from the infection itself, but rather from the pressure imbalances that occur in your sinuses during air travel. Sinuses are air-filled spaces in your skull that are normally connected to your nasal passages, allowing for air and mucus to flow freely. However, when you have a sinus infection, these pathways can become blocked due to inflammation and congestion. This blockage prevents the pressure in your sinuses from equalizing with the cabin pressure as the plane ascends and descends.
This article, based on expert advice from ENT specialists, will delve into the reasons behind sinus pain during flights and provide practical strategies to make your air travel more comfortable, even when you’re dealing with a sinus infection.
Why Sinus Infections and Flying Don’t Mix Well
The primary reason flying with a sinus infection hurts boils down to pressure changes. As an aircraft ascends and descends, the atmospheric pressure shifts dramatically. In healthy sinuses, air pressure adjusts seamlessly. But when sinus passages are blocked by infection-related swelling and mucus, this equalization process is disrupted.
 Woman pinching nose on plane, illustrating sinus pressure during flight with a sinus infection.
Woman pinching nose on plane, illustrating sinus pressure during flight with a sinus infection.
Imagine your sinuses as balloons within your skull. Normally, these balloons can inflate and deflate easily as external pressure changes. However, with a sinus infection, the pathways to these balloons become constricted. During ascent, the pressure in the cabin decreases, and the air in your sinuses tries to expand. If the sinus openings are blocked, this expansion causes pressure and pain. Conversely, during descent, the cabin pressure increases, and the air in your sinuses needs to compress. Again, if blocked, this compression leads to vacuum pressure and pain.
This pressure difference is the culprit behind the intense pain experienced when flying with a sinus infection. Similar pressure issues can occur in your ears, as the Eustachian tubes, which connect the middle ear to the back of the nose, can also become blocked by congestion, further compounding the discomfort.
To mitigate this pain, the goal is to relieve the blockage in your sinus passages and Eustachian tubes, allowing for proper pressure equalization. Here are four effective strategies recommended by ENT doctors.
4 Tips to Ease Sinus Pain When Flying
If you absolutely must fly with a sinus infection, these tips can help alleviate the pressure and pain, making your journey more bearable.
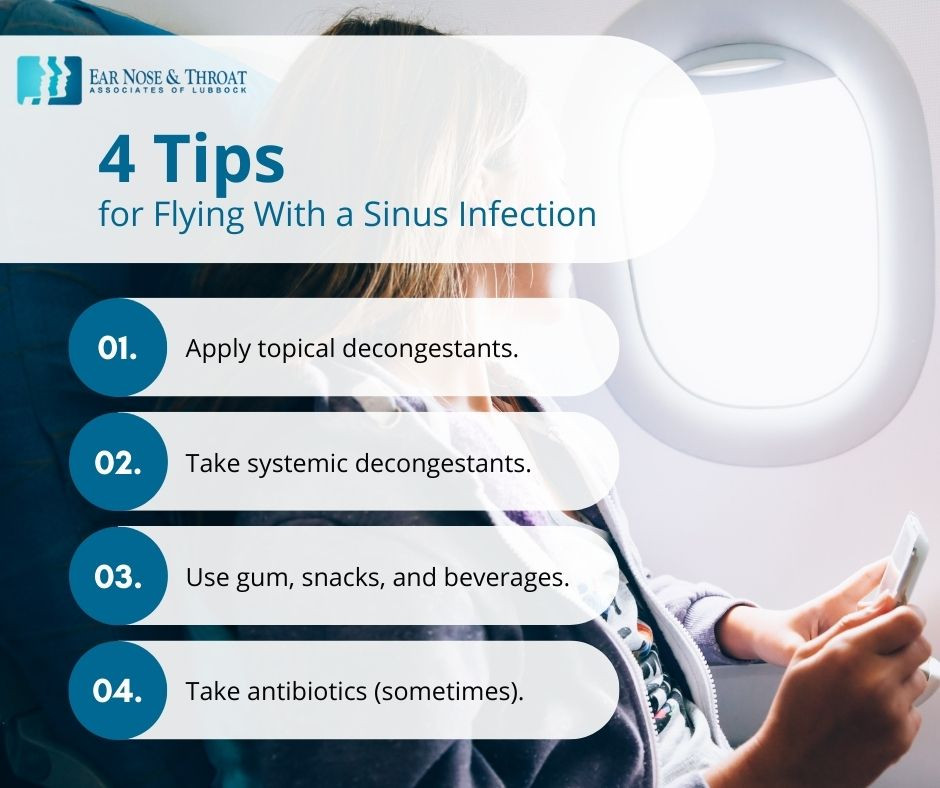 Infographic: 4 Tips for Flying With a Sinus Infection, including Topical Decongestants, Systemic Decongestants, Gum/Snacks/Beverages, and Antibiotics.
Infographic: 4 Tips for Flying With a Sinus Infection, including Topical Decongestants, Systemic Decongestants, Gum/Snacks/Beverages, and Antibiotics.
1. Utilize Topical Nasal Decongestants
Topical decongestants, typically in the form of nasal sprays, offer rapid relief from nasal congestion. These over-the-counter medications work directly in your nasal passages to shrink swollen blood vessels, effectively opening up sinus drainage pathways.
For air travel, using a topical decongestant approximately 30 minutes before takeoff can be particularly beneficial. This allows the medication to take effect and help clear your sinuses before the pressure changes become significant. Popular options include oxymetazoline (Afrin) and phenylephrine sprays. Saline nasal sprays or rinses can also be helpful in moisturizing nasal passages and thinning mucus, promoting drainage, and are a gentler alternative for some individuals.
However, it’s crucial to use topical decongestants sparingly. Prolonged use, typically beyond three days, can lead to rebound congestion, where nasal congestion worsens after the medication wears off. Reserve these sprays for your flight and consider other long-term congestion management strategies if needed.
2. Consider Systemic Decongestants
Systemic decongestants, available as oral pills or liquids, provide another avenue for reducing sinus congestion. These medications, such as pseudoephedrine and phenylephrine, work by constricting blood vessels throughout the body, including in the nasal passages. This systemic effect can help reduce swelling and open up both sinus passages and Eustachian tubes.
Common brand names containing systemic decongestants include Sudafed, Allegra-D, and Claritin-D. These can be taken a few hours before your flight to allow them to become effective before pressure changes occur.
However, systemic decongestants are not suitable for everyone. Individuals with high blood pressure, heart conditions, or certain other medical conditions should avoid them due to potential cardiovascular side effects. If you have any underlying health concerns, consult your doctor before using systemic decongestants. Exploring home remedies for sinus infections might be a safer alternative in such cases.
3. Chew Gum, Snack, and Hydrate
Simple actions like chewing gum, eating snacks, and drinking beverages can surprisingly aid in equalizing pressure in your ears and sinuses during a flight. The act of chewing and swallowing frequently encourages the opening of the Eustachian tubes. This opening allows air to flow into or out of the middle ear, balancing the pressure.
While chewing gum primarily targets ear pressure, the swallowing action associated with eating and drinking can also indirectly benefit sinus pressure by promoting overall drainage in the nasal passages. Staying hydrated by drinking water or juice can help thin mucus secretions, making them easier to drain from your sinuses.
Keep gum, healthy snacks, and a water bottle readily accessible during takeoff and landing to utilize this simple yet effective technique.
4. Antibiotics: When They Might Help (Before You Fly)
If you have a bacterial sinus infection and an upcoming flight, antibiotics might be beneficial if started well in advance of your travel date. Antibiotics are only effective against bacterial infections, not viral ones, and most sinus infections are viral.
A bacterial sinus infection is typically suspected when symptoms persist beyond 10 days and include significant facial pain, headache, and fever. In such cases, a doctor may prescribe antibiotics. However, antibiotics are not a quick fix and require several days to become fully effective.
If you suspect a bacterial sinus infection and have an impending flight, consult your doctor promptly. They can assess your condition, determine if antibiotics are appropriate, and prescribe them if necessary. Starting antibiotics early enough before your flight might help reduce the severity of your sinus infection and associated in-flight pain. It’s important to note that antibiotics are not a preventative measure to be taken just for flying; they are treatment for a bacterial infection diagnosed by a medical professional.
Confirm It’s a Sinus Infection Before You Fly
It’s crucial to correctly identify the cause of your symptoms before concluding you have a sinus infection, especially before flying. Symptoms of sinus infections can overlap with those of colds, flu, COVID-19, and allergies. Accurate self-diagnosis can be challenging.
Flying when contagious, regardless of whether it’s a sinus infection, cold, or flu, is generally discouraged to prevent spreading illness to fellow passengers. Moreover, some conditions might require different management approaches than a typical sinus infection.
If your symptoms persist for more than a week to ten days, or if they are severe, seeking medical advice is recommended. A doctor can accurately diagnose your condition and recommend the most appropriate treatment plan, ensuring both your comfort during travel and your overall health.

Philip Scolaro, MD: Leading Otolaryngologist at ENT Lubbock
Dr. Philip Scolaro is a highly respected board-certified Otolaryngologist serving the South Plains region. With over three decades of experience in Lubbock, Dr. Scolaro is renowned for his surgical expertise. He is the Medical Director for Covenant High Plains Surgery Center campuses, a valued member of Covenant Health Partners, and an adjunct faculty professor at Texas Tech University Health Sciences Center School of Medicine. Learn more about Dr. Scolaro and his expertise in ENT care.

David Cuthbertson, MD: Board-Certified ENT Specialist
Dr. David Cuthbertson is a dedicated physician at Ear Nose & Throat Associates of Lubbock. Joining ENT Lubbock after serving as chief resident at Baylor College of Medicine’s prestigious Bobby R. Alford Department of Otolaryngology in Houston, Dr. Cuthbertson is board certified in Otolaryngology and Head & Neck Surgery. He is recognized for his surgical skills, compassionate patient care, and proficiency in the latest ENT advancements. Discover more about Dr. Cuthbertson’s approach to patient-centered ENT care.