Deep vein thrombosis (DVT), a condition characterized by blood clots forming in deep veins, most commonly in the legs, is a serious health concern. A major complication of DVT is pulmonary embolism (PE), where a clot breaks loose and travels to the lungs, potentially causing severe consequences, including death. Both DVT and PE are collectively known as venous thromboembolism (VTE) and are typically treated with blood thinners (anticoagulants). Understanding VTE, its risks, and implications for travel, especially air travel, is crucial for affected individuals. One common question that arises for patients diagnosed with DVT is: How Long After A Dvt Can You Fly?
This article aims to provide a comprehensive guide to air travel after a DVT diagnosis, drawing upon medical insights and guidelines to ensure patient safety and informed decision-making.
Understanding DVT and VTE
Venous thromboembolism (VTE) is the overarching term for blood clots that occur in veins. As mentioned, it encompasses both deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT specifically refers to a blood clot in a deep vein, often in the legs, but it can occur in other parts of the body as well. When this clot dislodges and travels to the lungs, it becomes a pulmonary embolism (PE).
| Abbreviation | Term | Definition |
|---|---|---|
| DVT | Deep vein thrombosis | A clot in a deep vein, most commonly in the legs |
| PE | Pulmonary embolism | A clot that has traveled to the lungs |
| VTE | Venous thromboembolism | DVT or PE |
| CTEPH | Chronic thromboembolic pulmonary hypertension | Increased pressure in the vessels in the lung and stress on the heart |
| PTS | Post-thrombotic syndrome | A term used to describe long-term symptoms in the leg following a DVT |
| DOAC | Direct oral anticoagulant | A type of blood-thinning medication |
| – | Anticoagulant | Blood-thinning medication |
| – | Thrombophilia | Condition that makes one more likely to develop blood clots |
Blood clots form due to various risk factors, often a combination of them. These factors can be broadly categorized and are summarized in Figure 1. Sometimes, clots occur without identifiable reasons, termed ‘unprovoked’ or idiopathic clots.
Figure 1. Risk factors contributing to the formation of blood clots, including deep vein thrombosis (DVT) and pulmonary embolism (PE).
Blood clots can develop in deep veins, which are located deeper within the body and are more serious, or in superficial veins, which are closer to the skin. They can also be proximal, near major veins, or distal, in smaller veins further away from the center of the body. Figure 2 illustrates common superficial and deep veins in the arms and legs where clots may form. The location of a clot is crucial for assessing complication risks and determining the duration of anticoagulant treatment.
Figure 2. Illustration of superficial and deep veins in the leg and arm, indicating potential sites for blood clot formation.
DVT Diagnosis and Initial Steps
Upon diagnosis of DVT or PE, the subsequent steps depend on individual medical history, age, and the specific circumstances of the clot. Initial blood tests are crucial to evaluate anemia and kidney function. These tests help determine the suitability of different blood thinner medications (anticoagulants) and identify potential risks associated with their use. Choices of blood thinners include oral pills and injectable drugs, with warfarin and direct oral anticoagulants (DOACs) being commonly prescribed. Factors like kidney function, bleeding risks, and medication costs influence the selection of the most appropriate anticoagulant. Figure 3 provides a comparison between warfarin and DOACs.
Figure 3. A comparison of warfarin and direct oral anticoagulants (DOACs), two commonly prescribed blood thinners, highlighting their similarities and differences.
Routine cancer screenings, appropriate for age, are often recommended after a VTE diagnosis. Thrombophilia testing, which checks for clotting disorders, may be considered based on patient preference, impact on treatment, and cost. In some cases, familial testing for clotting disorders might also be evaluated depending on thrombophilia test results.
Specialist Care for Blood Clots
The type of medical specialist required for DVT or PE management varies. A primary care physician can guide patients to the necessary specialty care, which might include a vascular medicine specialist or a hematologist. In severe cases, interventional vascular specialists like interventional cardiologists, radiologists, or vascular surgeons may be involved. Thrombosis or Vascular Clinics, if available, and specialized Anticoagulation Clinics for warfarin management can also be beneficial.
Treatment and Duration of Anticoagulation
Anticoagulants are the standard treatment for DVT and PE. These medications work by slowing down blood clotting, preventing new clots, and stopping existing clots from growing. They allow the body to naturally dissolve the clot over time.
The duration of anticoagulation varies based on clot location and contributing factors. Superficial or distal clots may require no or short-term anticoagulation (weeks), while proximal clots or PE usually need at least 3 months of treatment. Longer treatment duration depends on the reasons behind the clot formation, as shown in Figure 4. Provoked clots, caused by temporary risk factors, might be treated for 3–6 months. Unprovoked clots or those due to persistent risks (e.g., cancer, immobility, clotting disorders) may necessitate long-term anticoagulation to prevent recurrence. Recurrent clots often require long-term therapy, considering previous triggers and bleeding risks. Patient preference regarding long-term blood thinners also plays a role. Regular follow-ups (e.g., annually) are crucial for those on long-term anticoagulants to reassess treatment, discuss new research, and review lab work.
Figure 4. The recurrence triangle, a tool to guide the duration of blood thinner treatment based on the cause of VTE and patient sex, aiding in deciding between short-term and long-term anticoagulation.
Physical Activity and Travel Post-DVT/PE
While rest is important during recovery, physical activity is encouraged after DVT or PE diagnosis as tolerated. Avoid pushing through pain or breathlessness. If feeling well enough, exercise and work are generally safe. However, high-risk activities with potential for injury should be avoided while on blood thinners due to increased bleeding risk. Medical alert bracelets or tags are advisable for those on anticoagulants.
Regarding air travel after DVT, there are no definitive guidelines for immediate flight safety. It is often recommended to avoid flying for the first 4 weeks after a DVT diagnosis, but this is not a strict rule. It’s essential to discuss individual risks and benefits with a healthcare provider before flying. Concerns about deep massage on the affected limb in the initial weeks after DVT exist due to the theoretical risk of clot dislodgement and PE. Gentle massage is acceptable later while on blood thinners, but deep tissue massage that could cause bruising should be avoided.
Symptom Improvement and Long-Term Risks
Symptoms like shortness of breath, chest pain, and leg pain/swelling typically improve gradually and often resolve completely. The highest risk period for serious complications is within the first few days after diagnosis, particularly the risk of PE. Most individuals experience noticeable improvement within days to weeks of starting anticoagulants and complete symptom resolution within 3 months. However, some may experience long-term symptoms.
Despite most patients fully recovering from DVT/PE, long-term issues such as post-thrombotic syndrome (PTS) after DVT or post-PE syndrome after PE can occur. In severe lung damage cases, chronic thromboembolic pulmonary hypertension (CTEPH) might develop.
Post-Thrombotic Syndrome (PTS)
PTS affects about 40% of DVT patients, causing chronic leg symptoms ranging from mild to severe, including swelling, pain, skin changes, and ulcers in severe cases. Compression stockings can alleviate PTS symptoms by improving fluid circulation in the legs.
Post-PE Syndrome
Post-PE syndrome involves persistent shortness of breath and chest discomfort even without significant lung damage or pulmonary hypertension, potentially impacting quality of life.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
CTEPH occurs when lung blood clots do not resolve, leading to chronic lung damage, increased lung vessel pressure, and heart strain. Worsening shortness of breath, especially during exertion, is a key symptom. Diagnostic steps for CTEPH include echocardiogram and lung scans, potentially requiring pulmonologist referral.
Emotional Well-being After DVT/PE
DVT or PE diagnosis can be emotionally challenging, causing shock, anxiety, and fear of recurrence. Temporary anxiety or low mood is normal initially, but persistent feelings may require professional mental health support. Support groups can be beneficial (Table 2).
| Organization and website | Type of resource |
|---|---|
| National Blood Clot Alliance www.stoptheclot.org | Patient information resource and national advocacy organization |
| North American Thrombosis Forum https://thrombosis.org/patients/ | Patient information resource |
| Anticoagulation Forum https://acforum.org/web/clinics.php | Listing of anticoagulation clinics |
Table 2. Resources for patients newly diagnosed with thrombosis, offering support and information.
Flying After DVT: Key Considerations and Recommendations
Returning to the primary question, “How long after a DVT can you fly?” While a definitive waiting period isn’t universally established, here are key considerations and recommendations:
- Initial 2-4 Weeks Post-DVT: Exercise Caution: It is generally advisable to avoid air travel for at least 2 to 4 weeks after being diagnosed with a DVT. This period is crucial for initial treatment to stabilize the condition and reduce the immediate risk of PE.
- Consult Your Doctor: The most important step before flying after a DVT is to consult your doctor. They can assess your individual situation, including the location and severity of your DVT, your overall health, and any ongoing treatment. Your doctor can provide personalized advice based on your specific circumstances.
- Stable Anticoagulation: Ensure that you are on a stable dose of anticoagulant medication and that your condition is well-managed before considering air travel. The medication needs time to become effective in preventing further clot formation or growth.
- Duration of Anticoagulation Therapy: If you are prescribed a short course of anticoagulants (e.g., 3-6 months for provoked DVT), it may be safer to fly once you have been on medication for a sufficient period and your doctor confirms it’s safe. For those on long-term anticoagulation, the risk assessment for flying might be different, and again, medical advice is crucial.
- Risk Factors for Recurrence: Your doctor will evaluate your risk factors for DVT recurrence. If you have ongoing risk factors, taking precautions during air travel becomes even more important.
- Travel Duration and Flight Length: Long-haul flights pose a higher risk of blood clot formation due to prolonged immobility. For shorter flights after the initial high-risk period, the risk may be lower, but this should still be discussed with your doctor.
Practical Tips for Safer Air Travel After DVT:
If your doctor clears you for air travel after a DVT, consider these precautions to minimize risks during your flight:
- Compression Stockings: Wear properly fitted compression stockings during flights. These help improve blood circulation in your legs and reduce the risk of clot formation.
- Stay Hydrated: Drink plenty of water and avoid excessive alcohol and caffeine, which can lead to dehydration and potentially increase clot risk.
- Regular Movement: Get up and walk around the cabin every 1-2 hours. If you are unable to walk, perform seated exercises like ankle pumps and calf raises to promote blood flow.
- Medication Management: Ensure you have an adequate supply of your anticoagulant medication for your trip and take it as prescribed. Carry your medication in your carry-on luggage in case of checked baggage delays.
- Medical Alert: Consider wearing a medical alert bracelet or carrying a card that indicates you are on blood thinners and have a history of DVT, in case of any medical emergencies during travel.
Conclusion
Managing DVT and understanding its implications for activities like air travel is vital for patient well-being. While there isn’t a fixed waiting period before flying after a DVT, a period of 2-4 weeks of avoidance is generally advised. The decision to fly should always be made in consultation with your healthcare provider, considering individual risk factors, treatment status, and the nature of travel. By taking appropriate precautions and following medical advice, individuals with a history of DVT can minimize risks and travel more safely.
Disclaimer: This article provides general information and should not be considered medical advice. Always consult with your healthcare provider for personalized guidance regarding air travel after a DVT diagnosis.
References
[1] Patient Information Page on DOACs.
[2] Thrombophilia testing.
[3] Factors contributing to blood clot formation.
[4] Patient Information Page on compression therapy.
[5] Spanish translation of this article.
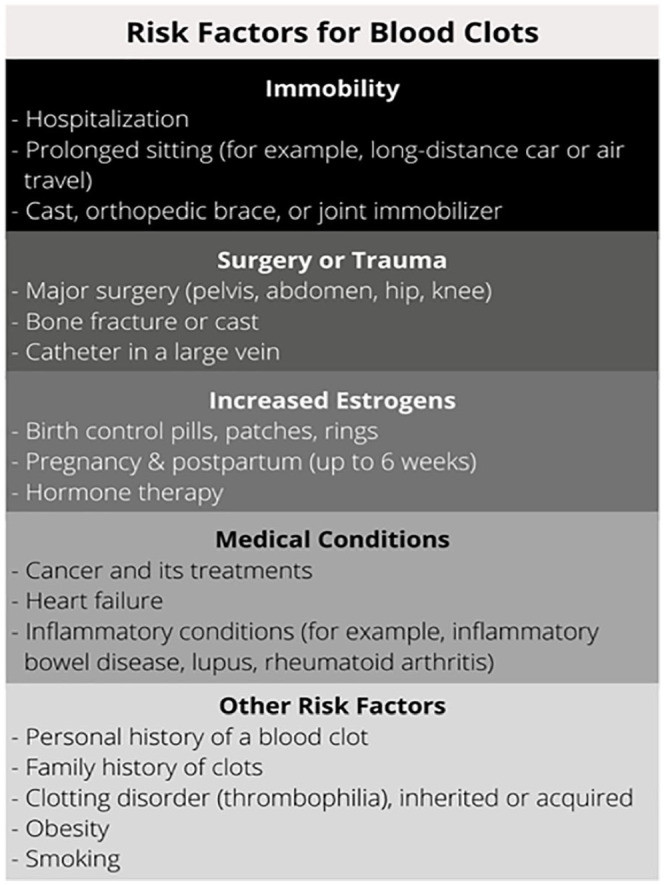
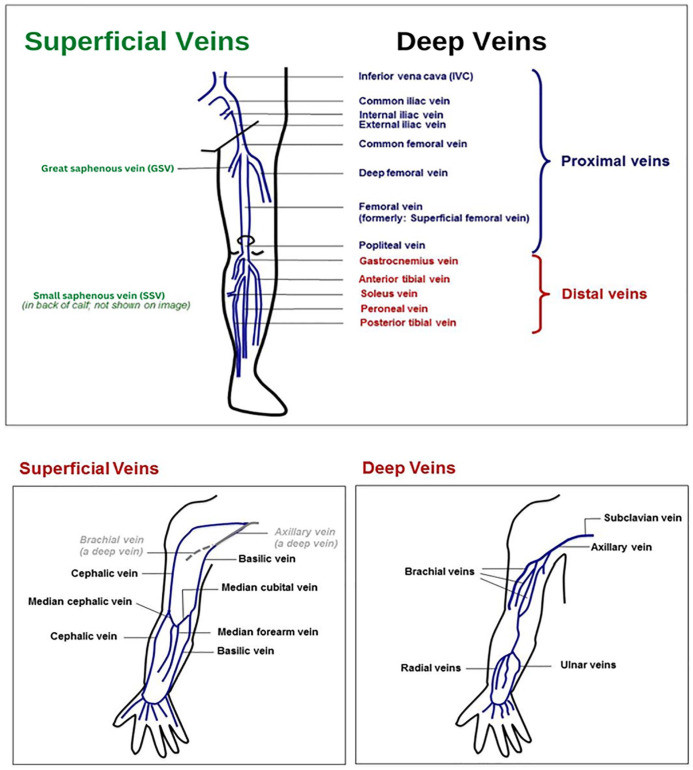 Figure 2.
Figure 2.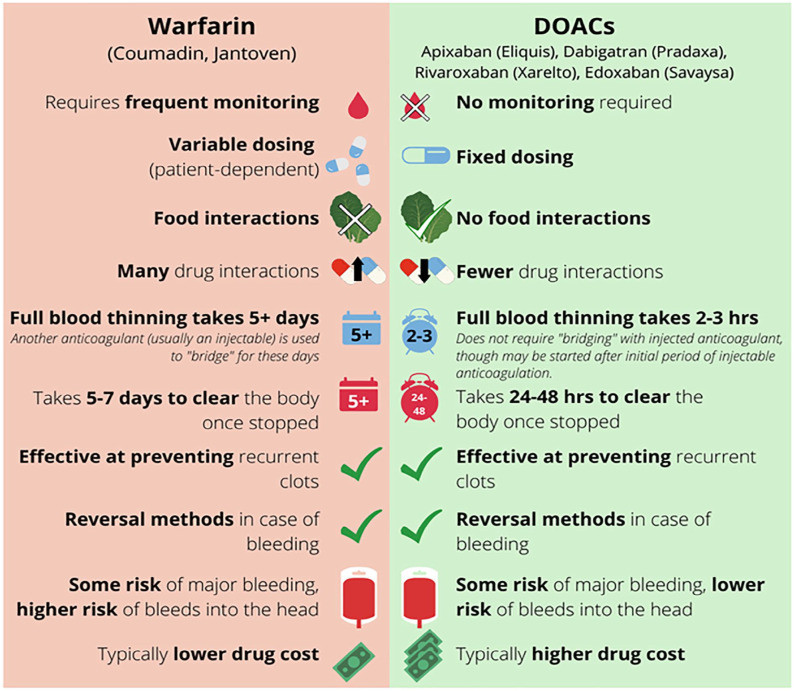 Figure 3.
Figure 3.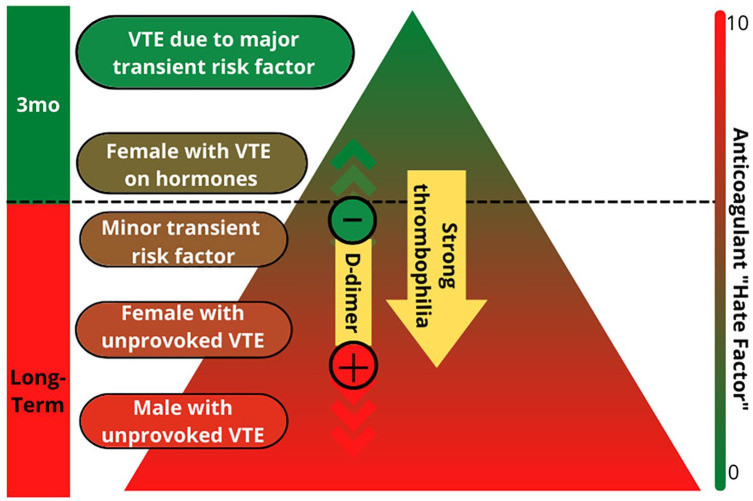 Figure 4.
Figure 4.